How Quickly Does HCG Rise? A Detailed Look at Early Pregnancy
For those embarking on the journey of pregnancy, understanding hormonal changes can be both empowering and reassuring. One of the most critical hormones in early pregnancy is human chorionic gonadotropin (hCG). The question, “How Quickly Does HCG Rise?” is a common one, reflecting a natural desire to ensure a healthy start. This article provides a comprehensive exploration of hCG levels, offering insights into what’s considered normal, what fluctuations might indicate, and the overall significance of monitoring hCG during the initial stages of pregnancy. We will delve into the nuances of hCG doubling times, factors that can influence hCG levels, and when it’s crucial to consult with a healthcare professional. Our goal is to provide you with the knowledge and understanding necessary to navigate this important aspect of early pregnancy with confidence.
Understanding the Basics of HCG and Early Pregnancy
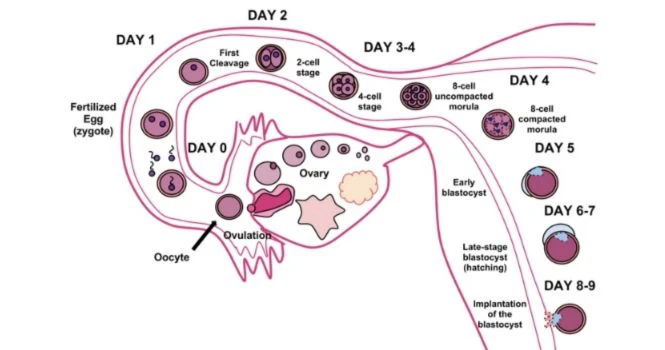
Human chorionic gonadotropin (hCG) is a hormone produced by the placenta shortly after implantation. Its primary role is to support the corpus luteum, which in turn produces progesterone, essential for maintaining the uterine lining and supporting the developing embryo. HCG levels are typically measured in milli-international units per milliliter (mIU/mL). The rise in hCG levels is a key indicator of a viable pregnancy, and monitoring its progression can provide valuable information about the health of the pregnancy.
The Role of HCG in Maintaining Pregnancy
HCG’s main job is to keep the pregnancy going in the early stages. By supporting the corpus luteum, it ensures that enough progesterone is produced until the placenta is fully developed and can take over progesterone production. Without adequate hCG, the uterine lining could break down, potentially leading to early pregnancy loss. Therefore, understanding the dynamics of hCG levels is crucial for assessing the viability of a pregnancy.
Normal HCG Levels in Early Pregnancy
HCG levels vary significantly from woman to woman, and even between pregnancies in the same woman. However, there are general ranges considered normal. Non-pregnant women typically have hCG levels below 5 mIU/mL. In early pregnancy, hCG levels usually start to rise rapidly, doubling approximately every 48 to 72 hours. This doubling time is a key indicator of a healthy pregnancy in the early weeks. However, it’s important to remember that these are just guidelines, and individual cases can vary.
How Quickly Does HCG Typically Rise? The Doubling Time
The doubling time of hCG is a critical metric used to assess the health of an early pregnancy. It refers to the time it takes for hCG levels to double in the bloodstream. This doubling time is most informative in the early weeks of pregnancy, typically between weeks 4 and 8 after the last menstrual period. After this point, the rate of increase usually slows down.
The 48-72 Hour Rule: What to Expect
As a general rule, hCG levels should double approximately every 48 to 72 hours in early pregnancy. This rapid increase indicates that the pregnancy is progressing as expected. However, it’s crucial to understand that this is just an average. Some healthy pregnancies may have slower doubling times, while others may have faster ones. The key is to look at the overall trend and consult with a healthcare provider for interpretation.
When Doubling Time Starts to Slow Down
Around 8 to 11 weeks of gestation, the rate of hCG increase naturally slows down. HCG levels typically peak around this time and then start to decline slightly. This is a normal part of pregnancy progression and is not usually a cause for concern. After the first trimester, hCG levels plateau and remain relatively stable for the remainder of the pregnancy.
Factors Affecting HCG Levels and Doubling Time
Several factors can influence hCG levels and doubling time, including:
- Gestational Age: HCG levels vary depending on how far along you are in your pregnancy.
- Multiple Pregnancies: Women carrying twins or multiples tend to have higher hCG levels than those carrying a single baby.
- Ectopic Pregnancy: In an ectopic pregnancy, where the fertilized egg implants outside the uterus, hCG levels may rise more slowly or not at all.
- Molar Pregnancy: A molar pregnancy, a rare complication, can cause abnormally high hCG levels.
- Miscarriage: A decline in hCG levels can be a sign of a potential miscarriage.
The Significance of Monitoring HCG Levels
Monitoring hCG levels can provide valuable insights into the health and viability of an early pregnancy. It is often used in conjunction with other tests, such as ultrasound, to confirm pregnancy and assess its progression. Serial hCG testing, which involves measuring hCG levels at intervals of 48 to 72 hours, is particularly useful in certain situations.
When Serial HCG Testing is Recommended
Serial hCG testing is typically recommended in the following situations:
- Suspected Ectopic Pregnancy: If there is a suspicion of ectopic pregnancy, serial hCG testing can help determine whether the pregnancy is progressing normally.
- Bleeding or Cramping: In cases of bleeding or cramping in early pregnancy, serial hCG testing can help assess the risk of miscarriage.
- In Vitro Fertilization (IVF): Serial hCG testing is often used in IVF pregnancies to monitor the early stages of development.
- History of Miscarriage: Women with a history of miscarriage may undergo serial hCG testing to monitor subsequent pregnancies more closely.
Interpreting HCG Results: What Do the Numbers Mean?
Interpreting hCG results requires careful consideration of several factors, including the gestational age, the rate of increase, and the presence of any symptoms. A single hCG value is less informative than a series of values measured over time. If hCG levels are not rising as expected, or if they are declining, it may indicate a problem with the pregnancy. However, it’s important to remember that there is a wide range of normal values, and individual cases can vary. Your doctor will consider your specific situation when interpreting your hCG results.
What HCG Tests Reveal About Pregnancy Viability
HCG tests are a cornerstone in assessing pregnancy viability, offering critical insights into the health and progression of an early pregnancy. By monitoring the hormone’s levels and their rate of change, healthcare providers can identify potential issues and ensure timely intervention when necessary. But what specific details do these tests reveal, and how can they help gauge the likelihood of a successful pregnancy?
Distinguishing Between Viable and Non-Viable Pregnancies
One of the primary functions of hCG testing is to differentiate between viable and non-viable pregnancies. A viable pregnancy is one that is developing normally and has a high likelihood of continuing to full term. In such cases, hCG levels typically rise steadily and predictably, doubling approximately every 48 to 72 hours in the early weeks. On the other hand, a non-viable pregnancy, such as an ectopic pregnancy or a miscarriage, often exhibits abnormal hCG patterns. In these situations, hCG levels may rise slowly, plateau, or even decline.
Identifying Potential Problems Early On
Serial hCG testing allows healthcare providers to identify potential problems early in the pregnancy. By measuring hCG levels at regular intervals, they can detect deviations from the expected doubling time and investigate the underlying cause. For example, a slow rise in hCG levels may indicate an ectopic pregnancy, which requires prompt medical attention to prevent serious complications. Similarly, a decline in hCG levels may suggest a miscarriage, allowing for timely management and support.
Ruling Out Ectopic Pregnancies
Ectopic pregnancies, where the fertilized egg implants outside the uterus, are a major concern in early pregnancy. HCG testing plays a crucial role in ruling out this condition. In ectopic pregnancies, hCG levels often rise more slowly than expected or may not rise at all. By monitoring hCG levels and performing an ultrasound, healthcare providers can usually diagnose ectopic pregnancies early on and provide appropriate treatment, such as medication or surgery.
Predicting Miscarriage Risk
HCG testing can also help predict the risk of miscarriage. A decline in hCG levels is often a sign of a failing pregnancy and may indicate an impending miscarriage. However, it’s important to note that a single hCG value is not sufficient to diagnose a miscarriage. Healthcare providers typically rely on serial hCG testing and ultrasound to confirm the diagnosis.
Comparing HCG Monitoring to Other Early Pregnancy Tests
While hCG monitoring is a valuable tool for assessing early pregnancy, it’s important to understand how it compares to other tests used during this critical period. Each test offers unique insights, and healthcare providers often use a combination of methods to gain a comprehensive understanding of the pregnancy’s health and progression. Let’s explore how hCG monitoring stacks up against other common early pregnancy tests.
HCG Blood Tests vs. Urine Tests
HCG can be detected in both blood and urine, but there are key differences between these two types of tests. Blood tests are generally more sensitive and accurate than urine tests, as they can detect lower levels of hCG. This means that blood tests can often confirm pregnancy earlier than urine tests, sometimes as early as 6 to 8 days after ovulation. Urine tests, on the other hand, are less sensitive and may not show a positive result until after a missed period. Blood tests also provide a quantitative measurement of hCG levels, allowing healthcare providers to track their rise over time. Urine tests, in contrast, only provide a qualitative result (positive or negative).
HCG Monitoring vs. Early Ultrasound
HCG monitoring and early ultrasound are complementary tools for assessing early pregnancy. HCG monitoring provides information about the hormonal environment, while ultrasound provides a visual image of the developing embryo. Early ultrasound can confirm the presence of a gestational sac in the uterus, rule out ectopic pregnancy, and assess the embryo’s heartbeat. However, ultrasound is typically not performed until hCG levels reach a certain threshold (usually around 1,500 to 2,000 mIU/mL), as it may not be able to detect a pregnancy earlier than this. HCG monitoring can be used to track the rise in hCG levels before ultrasound is performed, providing early clues about the pregnancy’s viability.
Progesterone Level Testing
Progesterone is another hormone that plays a crucial role in early pregnancy. Progesterone level testing is sometimes used in conjunction with hCG monitoring to assess the health of the pregnancy. Low progesterone levels may indicate a problem with the pregnancy, such as an ectopic pregnancy or a miscarriage. Progesterone supplementation may be recommended in some cases to support the pregnancy. However, progesterone level testing is not as commonly used as hCG monitoring, as hCG levels are generally considered a more reliable indicator of pregnancy viability.
Expert Review: The Advantages of Consistent HCG Monitoring
Consistent hCG monitoring offers several significant advantages in the early stages of pregnancy. From providing early confirmation to detecting potential complications, this practice can greatly enhance the chances of a healthy and successful pregnancy. Based on expert consensus and clinical experience, here’s an in-depth look at the benefits of consistent hCG monitoring.
Early Pregnancy Confirmation
One of the primary advantages of consistent hCG monitoring is its ability to confirm pregnancy early on. By detecting even small amounts of hCG in the blood, these tests can provide a positive result as early as 6 to 8 days after ovulation. This early confirmation can be particularly beneficial for women undergoing fertility treatments or those with a history of miscarriage, allowing them to receive timely medical care and support.
Accurate Gestational Age Estimation
Consistent hCG monitoring can also help estimate the gestational age of the pregnancy more accurately. By tracking the rise in hCG levels over time, healthcare providers can determine how far along the pregnancy is and ensure that it is progressing at the expected rate. This information is crucial for scheduling prenatal appointments, performing screening tests, and planning for delivery.
Detecting Ectopic Pregnancies
Ectopic pregnancies, where the fertilized egg implants outside the uterus, are a serious complication that requires prompt medical attention. Consistent hCG monitoring can help detect ectopic pregnancies early on, allowing for timely intervention and preventing potentially life-threatening complications. In ectopic pregnancies, hCG levels often rise more slowly than expected or may not rise at all. By monitoring hCG levels and performing an ultrasound, healthcare providers can usually diagnose ectopic pregnancies early on and provide appropriate treatment.
Identifying Potential Miscarriage Risks
Consistent hCG monitoring can also help identify potential miscarriage risks. A decline in hCG levels is often a sign of a failing pregnancy and may indicate an impending miscarriage. However, it’s important to note that a single hCG value is not sufficient to diagnose a miscarriage. Healthcare providers typically rely on serial hCG testing and ultrasound to confirm the diagnosis. By identifying potential miscarriage risks early on, healthcare providers can provide appropriate support and counseling to women and their families.
Personalized Pregnancy Care
Consistent hCG monitoring allows for personalized pregnancy care tailored to each woman’s unique needs and circumstances. By tracking hCG levels and other relevant markers, healthcare providers can gain a comprehensive understanding of the pregnancy’s health and progression and provide individualized recommendations for prenatal care, nutrition, and lifestyle modifications.
Addressing Potential Limitations of HCG Monitoring
While consistent hCG monitoring offers numerous advantages, it’s important to acknowledge its potential limitations. Here are some points to consider:
- Variability in HCG Levels: HCG levels can vary significantly between women and even between pregnancies in the same woman. This variability can make it challenging to interpret hCG results and may lead to unnecessary anxiety or interventions.
- False Positives and False Negatives: HCG tests are generally accurate, but false positives and false negatives can occur. False positives may be caused by certain medical conditions or medications, while false negatives may occur if the test is performed too early in the pregnancy.
- Cost and Inconvenience: Consistent hCG monitoring can be costly and inconvenient, as it requires multiple blood draws and frequent visits to the healthcare provider.
What To Do With Your HCG Level Information
Understanding how quickly hCG rises during early pregnancy is crucial, but knowing what to do with that information is equally important. Whether your levels are within the typical range or show some variation, here’s a guide on how to proceed and make informed decisions.
Consulting with Your Healthcare Provider
The first and most important step is to consult with your healthcare provider. They can interpret your hCG results in the context of your overall health history, symptoms, and other test results. Your healthcare provider can also provide personalized recommendations for further testing or treatment, if necessary.
Understanding the Range of Normal
It’s important to remember that there is a wide range of normal hCG levels in early pregnancy. What is considered normal for one woman may not be normal for another. Your healthcare provider can help you understand what is considered normal for you, based on your individual circumstances.
Following Your Doctor’s Recommendations
Once you have consulted with your healthcare provider, it’s important to follow their recommendations carefully. This may include further testing, such as serial hCG testing or ultrasound, or it may involve lifestyle modifications or medical treatments. Your healthcare provider will work with you to develop a plan that is tailored to your specific needs and circumstances.
Managing Stress and Anxiety
The early stages of pregnancy can be a stressful and anxious time, especially if you are experiencing any complications or concerns. It’s important to manage your stress and anxiety levels by practicing relaxation techniques, such as deep breathing, meditation, or yoga. You may also find it helpful to talk to a therapist or counselor, or to join a support group for pregnant women.
Maintaining a Healthy Lifestyle
Maintaining a healthy lifestyle is crucial for a healthy pregnancy. This includes eating a balanced diet, getting regular exercise, and avoiding smoking, alcohol, and illicit drugs. Your healthcare provider can provide you with specific recommendations for a healthy lifestyle during pregnancy.
Navigating Early Pregnancy with Confidence
Understanding how quickly hCG rises is a crucial aspect of monitoring early pregnancy. While fluctuations and variations can cause anxiety, remember that a healthcare provider is your best resource for accurate interpretation and personalized guidance. By staying informed, communicating openly with your doctor, and focusing on a healthy lifestyle, you can navigate the early stages of pregnancy with greater confidence and peace of mind. This knowledge empowers you to be an active participant in your prenatal care, ensuring the best possible outcome for you and your baby. Remember, every pregnancy is unique, and your healthcare team is there to support you every step of the way.
</n
