Dietary Strategies for Managing Dystonia: Foods to Avoid and Why
Dystonia, a neurological movement disorder characterized by involuntary muscle contractions, can significantly impact an individual’s quality of life. While there’s no cure, various treatments can help manage symptoms. Emerging research suggests that dietary modifications can play a supportive role in alleviating some symptoms and improving overall well-being. This comprehensive guide delves into the foods to avoid with dystonia, explaining the rationale behind these recommendations and providing actionable strategies for dietary management. We aim to empower individuals with dystonia and their caregivers with the knowledge to make informed dietary choices.
Understanding Dystonia and the Potential Role of Diet
Dystonia arises from malfunctions in the basal ganglia, a region of the brain responsible for motor control. This leads to sustained muscle contractions, causing twisting, repetitive movements, or abnormal postures. The severity and type of dystonia vary widely, affecting different parts of the body. While the exact causes are often unknown (idiopathic dystonia), genetics, other medical conditions, or medication side effects can contribute.
The connection between diet and dystonia is complex and still under investigation. However, certain foods and nutrients can influence neurotransmitter function, inflammation, and oxidative stress—all factors potentially implicated in dystonia. By understanding these connections, individuals may be able to fine-tune their diets to minimize symptom exacerbation.
Foods to Avoid or Limit with Dystonia: A Detailed Guide
While a universally applicable dystonia diet doesn’t exist, certain food groups and substances have been identified as potential triggers or contributors to symptom worsening. This section provides a detailed overview of these foods, along with the reasoning behind their potential impact.
1. Excessive Caffeine Intake
Caffeine, a stimulant found in coffee, tea, energy drinks, and chocolate, can exacerbate dystonia symptoms in some individuals. Caffeine stimulates the central nervous system, potentially increasing neuronal excitability and muscle spasticity. It can also interfere with certain medications used to manage dystonia.
Recommendation: Limit or avoid caffeine consumption. If you regularly consume caffeine, gradually reduce your intake to minimize withdrawal symptoms. Opt for decaffeinated beverages or herbal teas. Monitor your symptoms closely to determine your individual tolerance.
2. Artificial Sweeteners (Aspartame, Sucralose, Saccharin)
Artificial sweeteners, commonly found in diet sodas, sugar-free products, and processed foods, have been linked to neurological issues in some studies. Aspartame, in particular, has been reported to trigger or worsen symptoms in individuals with certain neurological conditions. The exact mechanisms are still under investigation, but some theories suggest that artificial sweeteners can affect neurotransmitter balance or contribute to excitotoxicity in the brain.
Recommendation: Eliminate or significantly reduce the consumption of artificial sweeteners. Read food labels carefully and opt for naturally sweetened alternatives like stevia, monk fruit, or small amounts of honey or maple syrup (if tolerated). Note that even natural sweeteners should be used in moderation.
3. Processed Foods High in Additives and Preservatives
Processed foods often contain a cocktail of additives, preservatives, artificial colors, and flavors that can potentially trigger adverse reactions in sensitive individuals. These substances can contribute to inflammation, oxidative stress, and neurological dysfunction. Monosodium glutamate (MSG), a common flavor enhancer, is a known excitotoxin that can overstimulate neurons.
Recommendation: Prioritize whole, unprocessed foods. Cook meals from scratch using fresh ingredients. Read food labels carefully and avoid products with long lists of artificial ingredients. Limit your intake of fast food, packaged snacks, and processed meats.
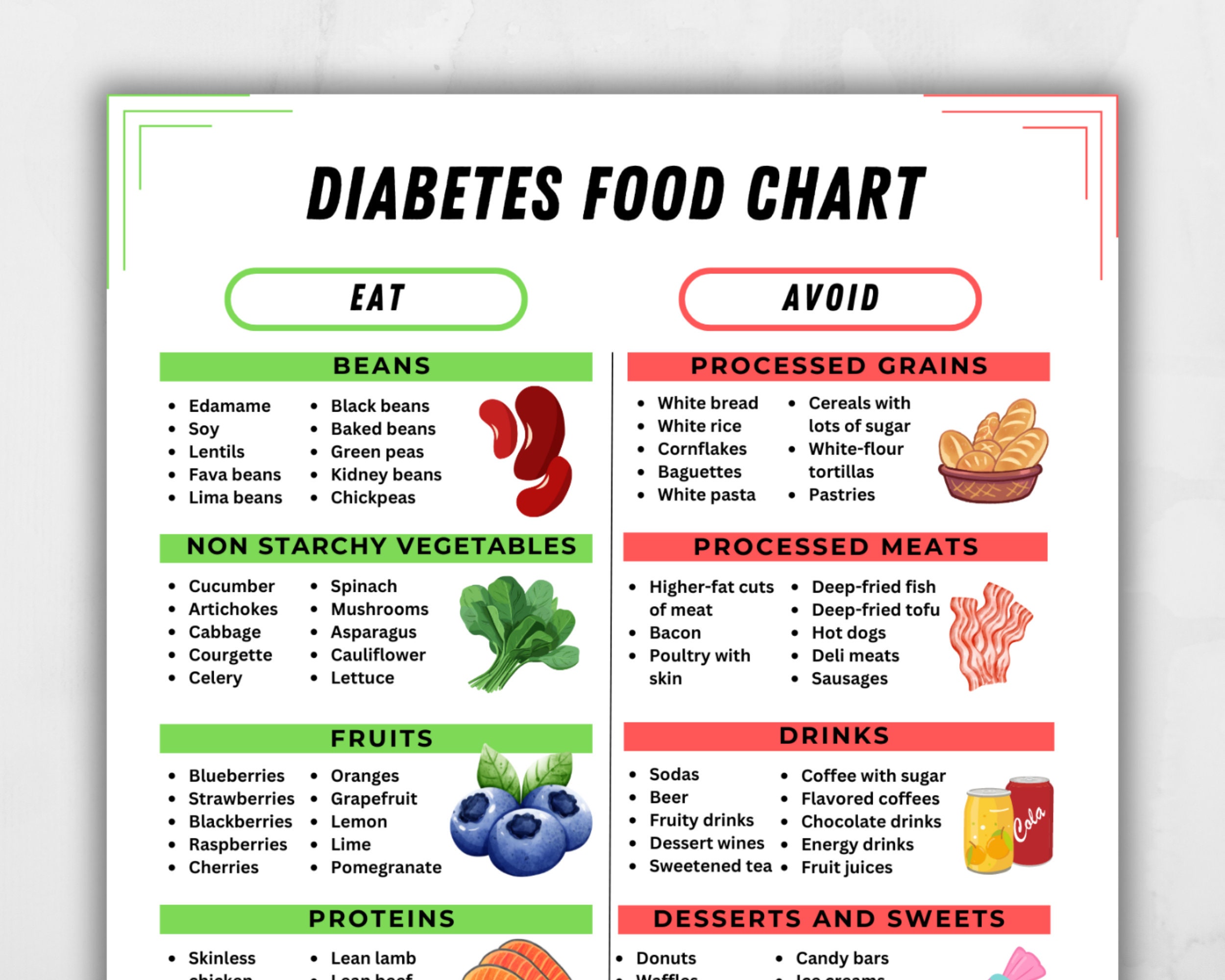
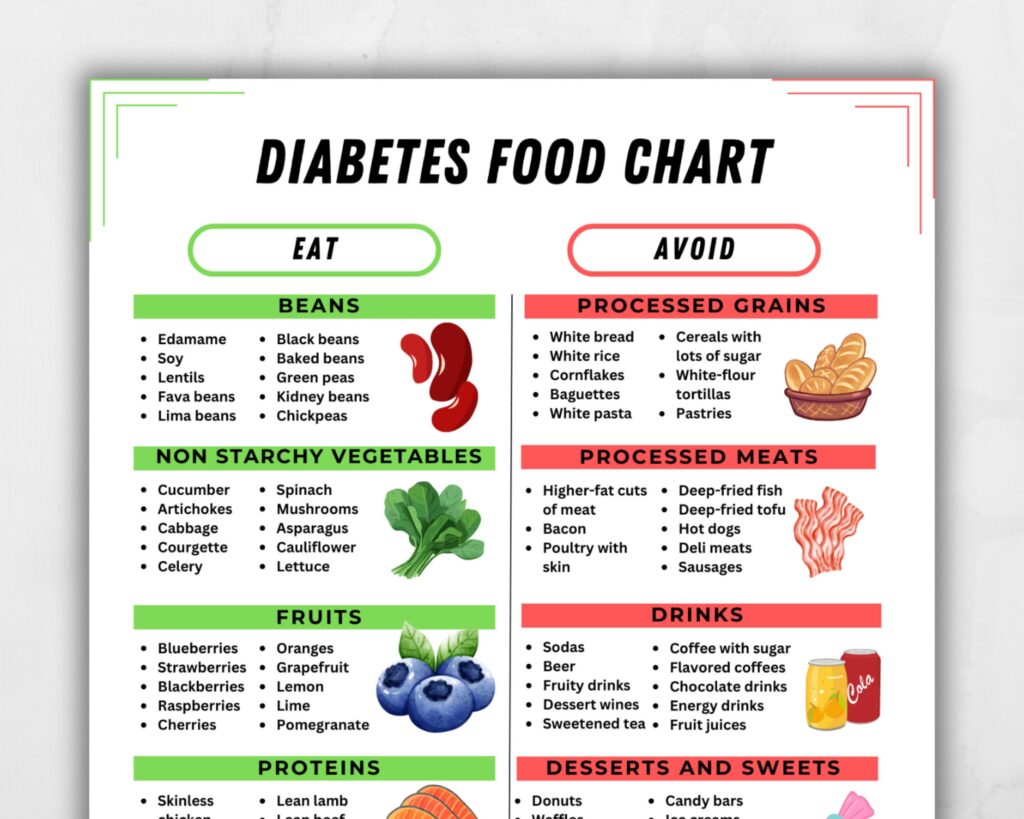
4. Refined Sugars and High-Glycemic Carbohydrates
Refined sugars and high-glycemic carbohydrates, such as white bread, pastries, and sugary drinks, can cause rapid spikes in blood sugar levels, leading to insulin resistance and inflammation. These fluctuations can negatively impact neurotransmitter function and potentially worsen dystonia symptoms.
Recommendation: Limit your intake of refined sugars and high-glycemic carbohydrates. Choose complex carbohydrates like whole grains, vegetables, and legumes. Focus on a balanced diet with adequate protein and healthy fats to stabilize blood sugar levels.
5. Alcohol
Alcohol is a neurotoxin that can impair brain function and worsen neurological symptoms. It can interfere with medications used to treat dystonia and disrupt sleep patterns, which are crucial for managing symptoms. Even moderate alcohol consumption can exacerbate muscle spasticity and coordination problems.
Recommendation: Avoid or strictly limit alcohol consumption. If you choose to drink alcohol, do so in moderation and under the guidance of your healthcare provider. Be aware of the potential interactions with your medications.
6. Foods High in Saturated and Trans Fats
Saturated and trans fats, commonly found in fried foods, processed snacks, and fatty meats, can contribute to inflammation and oxidative stress, potentially exacerbating dystonia symptoms. These fats can also impair blood flow to the brain and negatively impact neuronal function.
Recommendation: Limit your intake of saturated and trans fats. Choose lean protein sources, healthy fats like olive oil and avocado, and focus on a diet rich in fruits and vegetables. Avoid processed foods and fried foods.
7. Gluten (For Individuals with Gluten Sensitivity or Celiac Disease)
While not a universal trigger for all individuals with dystonia, gluten, a protein found in wheat, barley, and rye, can cause inflammation and neurological symptoms in those with gluten sensitivity or celiac disease. Gluten sensitivity can manifest with a variety of neurological symptoms, including muscle weakness, fatigue, and cognitive dysfunction. Celiac disease is an autoimmune disorder triggered by gluten, leading to damage to the small intestine.
Recommendation: If you suspect you may have gluten sensitivity or celiac disease, consult with your healthcare provider for testing. If diagnosed, strictly avoid gluten-containing foods. Opt for gluten-free alternatives like rice, quinoa, and gluten-free flours.
8. Dairy (For Individuals with Dairy Sensitivity or Lactose Intolerance)
Similar to gluten, dairy products can trigger inflammation and digestive issues in individuals with dairy sensitivity or lactose intolerance. These issues can indirectly affect neurological function and potentially worsen dystonia symptoms. Lactose intolerance is the inability to digest lactose, a sugar found in milk and dairy products.
Recommendation: If you suspect you may have dairy sensitivity or lactose intolerance, consult with your healthcare provider. If diagnosed, limit or avoid dairy products. Choose dairy-free alternatives like almond milk, soy milk, or coconut milk.
The Neurotransmitter Connection: How Diet Impacts Dystonia
Neurotransmitters, chemical messengers that transmit signals between nerve cells, play a crucial role in motor control. Imbalances in neurotransmitter levels can contribute to dystonia symptoms. Diet can influence neurotransmitter synthesis, release, and reuptake, potentially affecting the severity of dystonia.
For example, dopamine, a neurotransmitter involved in movement control, is often deficient in individuals with dystonia. Certain foods, such as those high in tyrosine, a precursor to dopamine, may help boost dopamine levels. Conversely, foods that deplete dopamine, such as refined sugars and processed foods, may worsen symptoms.
Serotonin, another neurotransmitter involved in mood regulation and sleep, can also be affected by diet. Deficiencies in serotonin can lead to anxiety, depression, and sleep disturbances, which can exacerbate dystonia symptoms. Foods rich in tryptophan, a precursor to serotonin, may help improve serotonin levels.
Crafting a Dystonia-Friendly Diet: Practical Tips and Strategies
Creating a dystonia-friendly diet involves a personalized approach, taking into account individual triggers, sensitivities, and nutritional needs. Here are some practical tips and strategies to guide you:
- Keep a Food Diary: Track your food intake and any associated symptoms to identify potential triggers.
- Focus on Whole, Unprocessed Foods: Prioritize fruits, vegetables, lean protein, and healthy fats.
- Cook Meals from Scratch: This allows you to control the ingredients and avoid harmful additives.
- Read Food Labels Carefully: Pay attention to ingredients, serving sizes, and nutritional information.
- Stay Hydrated: Drink plenty of water throughout the day to support optimal brain function.
- Consult with a Registered Dietitian: A registered dietitian can help you develop a personalized meal plan that meets your specific needs.
The Importance of Hydration and Electrolyte Balance
Proper hydration is essential for overall health and neurological function. Dehydration can exacerbate muscle spasticity and fatigue, potentially worsening dystonia symptoms. Electrolytes, such as sodium, potassium, and magnesium, play a crucial role in nerve and muscle function. Imbalances in electrolyte levels can contribute to muscle cramps, weakness, and other neurological issues.
Recommendation: Drink plenty of water throughout the day. Aim for at least eight glasses of water daily. Replenish electrolytes after exercise or during periods of excessive sweating. Consider electrolyte-rich beverages like coconut water or sports drinks (in moderation). Discuss electrolyte supplementation with your healthcare provider if necessary.
Navigating the Challenges of Dietary Changes
Making significant dietary changes can be challenging, especially when dealing with a chronic condition like dystonia. It’s important to approach these changes gradually and with a supportive mindset. Here are some tips for navigating the challenges:
- Start Small: Focus on making one or two changes at a time.
- Be Patient: It may take time to see noticeable improvements in your symptoms.
- Seek Support: Connect with other individuals with dystonia or join a support group.
- Celebrate Successes: Acknowledge and reward yourself for achieving your dietary goals.
Beyond Diet: A Holistic Approach to Dystonia Management
Diet is just one piece of the puzzle when it comes to managing dystonia. A holistic approach that incorporates other lifestyle factors, such as exercise, stress management, and sleep hygiene, can provide comprehensive symptom relief. Regular exercise can improve muscle strength, flexibility, and coordination. Stress management techniques, such as meditation and yoga, can help reduce muscle tension and anxiety. Adequate sleep is crucial for brain function and overall well-being.
Expert Insight: The Gut-Brain Connection in Dystonia
Emerging research highlights the intricate connection between the gut microbiome and brain health, often referred to as the gut-brain axis. The gut microbiome, the community of microorganisms living in the digestive tract, can influence neurotransmitter production, inflammation, and immune function. Disruptions in the gut microbiome have been linked to various neurological disorders, including dystonia.
Supporting a Healthy Gut Microbiome: Incorporate probiotic-rich foods like yogurt, kefir, and fermented vegetables into your diet. Consume prebiotic-rich foods like garlic, onions, and asparagus to nourish beneficial gut bacteria. Avoid processed foods, antibiotics (when not medically necessary), and other factors that can disrupt the gut microbiome.
Personalizing Your Dietary Approach
The ideal diet for managing dystonia is highly individual. What works for one person may not work for another. It’s essential to experiment, track your symptoms, and work closely with your healthcare team to develop a personalized dietary plan that meets your specific needs and goals. Factors such as age, gender, activity level, and other medical conditions can influence your dietary requirements.
The Future of Dietary Interventions for Dystonia
Research on the role of diet in dystonia is ongoing and rapidly evolving. Future studies may uncover new dietary strategies and personalized approaches for managing symptoms. Advances in understanding the gut-brain axis and the role of specific nutrients may lead to more targeted interventions. Staying informed about the latest research and working closely with your healthcare team can help you optimize your dietary approach.
Empowering Yourself Through Informed Dietary Choices
Navigating dystonia can be challenging, but understanding the potential impact of your diet can empower you to take control of your health. By making informed dietary choices, you can potentially alleviate symptoms, improve your overall well-being, and enhance your quality of life. Remember to consult with your healthcare provider or a registered dietitian before making any significant dietary changes. Your journey to better health starts with knowledge and a commitment to self-care. This guide provides a robust starting point, enabling you to actively participate in managing your dystonia through thoughtful nutrition and lifestyle adjustments.